- Review
- Open access
- Published:
Olfactory reference disorder—a review
Middle East Current Psychiatry volume 30, Article number: 95 (2023)
Abstract
Olfactory Reference Disorder (ORD) is a known clinical entity for several decades; however, it is only in ICD 11 that it has found its niche. Long considered a delusional disorder, it is currently classified as an obsessive–compulsive (OC) spectrum disorder.
ORD is characterised by an erroneous conviction that the body is emitting an unpleasant smell. Patients harbour referential thinking, practise rituals to eliminate or mask the perceived odour, and avoid social interactions. While the conviction can be at a delusional level in some patients, the preoccupation has an obsessive quality in others. The level of insight can be varied. Patients present to mental health settings after traversing a long pathway of care comprising of various specialists. Medical and psychiatric conditions which can present with ORD-like symptoms need to be ruled out. Establishing a therapeutic alliance is the first step in management. There are no randomised controlled trials comparing treatment options in ORD. Antidepressants, antipsychotics, and their combinations have been used with varying degrees of success, in addition to psychotherapy and electroconvulsive therapy. Data on prognosis is limited.
Introduction
Of the five senses that man is blessed with, smell, taste, and touch have always been accorded a backseat to sight and hearing. This applies to psychopathology as well where problems related to smell are often overlooked. A good example is that of olfactory reference disorder (ORD) or olfactory reference syndrome (ORS) as it used to be popularly called. Olfactory reference disorder is defined as a condition “in which one believes that his or her body emits a foul odour that makes people react in a negative way to their body” [1]. The presentation encompasses an overlapping phenomenology of overvalued ideas, delusions, somatic preoccupations, anxiety, and obsessive phenomena; hence, slotting it into a particular diagnostic category has been wrought with controversies. The theory that bodily odour is normal and that ORD may represent a higher intensity in its dimension has added to the confusion. ORD in its classical form or as an isolated body odour symptom of another disorder is a common clinical presentation. Though prevalence statistics for the disorder are available in literature, most studies also attach a disclaimer stating that these values are probably underestimated. Hence, the magnitude of this condition is presumably much higher than what is generally quoted. Patients suffer from intense embarrassment and personal distress and turn into social recluses because of ORD. There is also an associated risk of self-harm. Though the condition came to clinical attention several decades ago, our knowledge of the various treatment options remains restricted to case reports and case series. ORD has now been recognised as a prominent psychiatric condition and has found its niche in the recent versions of the classificatory systems.
The aim of this review is to provide an overview of olfactory reference disorder, covering the definition, evolution of the concept and classification, epidemiology, psychopathology and clinical features, comorbidities, diagnosis, differential diagnosis, assessment, treatment, and prognosis.
Evolution of the concept and classification
Descriptions of a clinical condition that resembles the current day ORS date to the 1800s, with cases being reported from Asia, Africa, the USA, Europe, and the Middle East. Several of these were then described as schizophrenia, though they did not meet the full criteria for the disorder. We owe the clinical description and the term olfactory reference syndrome to Pryse-Philips who proposed the same after analysing a large case series [1]. The condition has received several other monikers, chiefly, parosmia [2], hallucinations of smell [1], chronic olfactory paranoid syndrome [3], and monosymptomatic hypochondriacal psychosis [4]. It was predominantly conceptualised as a type of delusional disorder [5].
Despite the clear existence of ORS, it had not been classified separately as a disorder in the earlier versions of the International Classification of Diseases (ICD) or Diagnostic and Statistical Manual (DSM).
In the DSM IIIR, it is described as a common presentation of a “delusional disorder, somatic type”. The DSM IV TR and ICD 10 continued this tradition; the term ORS is not included in either of them. DSM IV makes a reference to ORS in the section on social phobia as well as under its culture-bound syndrome section, with specific mention of the Taijin Kyofusho of Japan [5].
However, a seminal paper that published a systematic review of 84 cases reported in existing literature, while supporting the existence of ORS, questioned its validity as a delusional disorder. The authors put forth the argument that while the conviction held by some patients (57%) amounts to a delusional level, not all cases are delusional (43%). They posited that the position of the ORS needs to be reconsidered in future classificatory systems [6].
Despite there being a proposal to include ORD as a separate disorder in the DSM 5, it only achieved a mention under the category “other specified obsessive–compulsive and related disorders”, with a specific mention of the culture-bound variant (Taijin Kyofusho).
ORD has finally come into its own in the ICD 11. It has merited a separate category with a code (6B22) under obsessive–compulsive and related disorders. Furthermore, it has been granted additional insight specifiers (fair to good, poor to absent insight and unspecified).
Another debate that has ranged since long is whether ORD must be classified categorically as a separate entity or conceptualised as a dimensional construct, considering its boundary with normal body odour concerns. One study that attempted to make this distinction assessed a mixed sample of 757 individuals (both community and student participants). Three independent taxometric procedures were conducted on three indicators derived from the Yale-Brown Obsessive–Compulsive Scale Modified for olfactory reference syndrome, namely, ORD obsessions, ORD compulsions, and avoidance. Two of the three revealed a dimensional rather than a categorical structure of ORD. The researchers suggested that in clinical practice, it would be better to view ORD as a dimensional concept while assessing and planning treatment [7].
Besides, though the neurobiology of ORD as a separate disorder has been poorly researched, an integrated neurobiological approach has been proposed [8]. ORD incorporates symptoms of various phenomenological types, and it is known that an overlapping circuitry is implicated in the neurobiology of trauma reactions, OCD, and psychotic spectrum disorders. This model also lends credence to the viewing of the ORD phenomenology as dimensional rather than categorical.
The classification of ORD has been summarised in Table 1.
Epidemiology
The community prevalence of olfactory reference disorder ranges from 0.5 to 2.1%; however, since most of these values are based on self-report of body odour concerns, it is probably a far from accurate value [5]. There appears to be underreporting from developing nations as well [9].
Women are affected more, in addition to single individuals. The onset is most often in the mid-twenties [6, 10], with some case reports suggesting an earlier age of onset [11].
The most frequently seen personality traits in these individuals (67%) correspond to the cluster C of the DSM (anxious, perfectionistic, and dependent) [6]. There is limited evidence to show that some of these patients may have a family history of schizophrenia [12].
Most patients reach a mental health setting only through a long pathway of care encompassing dentists, dermatologists, gastroenterologists, and, sometimes, even the surgical specialties [13, 14]. The delay in clinical care is due to the embarrassing nature of the symptom. If ORD is associated with poor or absent insight, it delays treatment seeking even further.
Psychopathology and clinical features
The core symptom in ORD is a preoccupation with the erroneous belief that one’s body is emitting an offensive smell. Phenomenologically, these beliefs range from overvalued ideas to delusions [15]. The constant preoccupation also has an obsessive quality to it. The patient describes the odour as foul. One or several body parts may be held responsible as the source of the odour, commonly reported ones being the mouth, axillae, feet, and genital regions. The source may change over time. Rarely, patients report of non-bodily odours such as that of ammonia [2] or detergent [16]. Sometimes, the patient may be unable to pinpoint an exact region as the source of smell. The odour is reported to be present all the time. Half of the patients complain of being able to smell the foul odour [6]. Insight may be varied. In the systematic review previously quoted, 49% of the reports mention a precipitating event/statement, which while appearing to be incongruous at the time seemed to set the patients on a morbid course. These were chiefly smell-related negative experiences (85%) and less often unrelated sources of stress (17%). Common examples reported by patients include “an older sibling quipping that his feet smelled, a colleague turning away once or twice during a conversation, housemates teasing her for breaking wind, had an episode of halitosis during a severe throat infection, etc.” [6].
In keeping with the name, the belief is also accompanied by referential ideas (74%) that are sometimes of a delusional intensity. They often misinterpret other peoples’ actions, e.g. a couple of colleagues sniffed or took their handkerchiefs out when he was nearby, she was gifted a perfume for her birthday by her classmates, a vacant seat next to her on a bus was not claimed by anybody though the bus was full, friends stopped talking soon as she appeared in the distance, hence they probably had been discussing that she stank, etc. [6].
As a result, these patients often suffer from intense social anxiety; they avoid close relationships and social contacts or endure them with high levels of embarrassment and distress. In severe cases, they may become house bound [6].
There are repeated behaviours aimed at checking for, camouflaging, or eliminating the odour that these patients perceive. These could include multiple baths, ritualistic grooming, using deodorants or powder excessively, chewing gum or mints, and making drastic changes in diet. These are often time consuming and add to the social and occupational dysfunction [12].
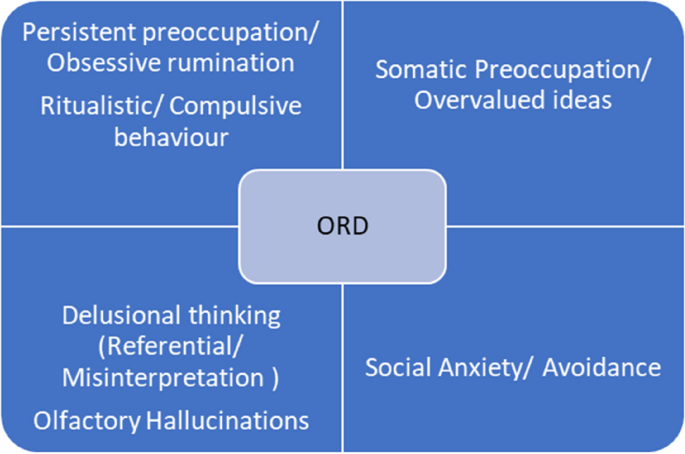
The range of psychopathology seen in ORD is summarised in Fig. 1.
A 2011 study of 20 patients diagnosed with ORD assessed them using semi structured measures to gather information about demographic and clinical features. Women constituted 60% of the sample, the mean age being 33.4 ± 14.1 years. The most common sources of the odour were reported from mouth (75%), armpits (60%), and genitals (35%). Delusional ORS beliefs and olfactory hallucinations were the most common (85%) followed by referential thinking (77%). Ninety-five percent of the patients reported repetitive behaviours. Fifty-three percent had undergone psychiatric hospitalisation for the symptoms, 68% reported suicidal ideation, while 32% had a history of attempts at self-harm. Forty-four percent had sought treatment from non-mental health specialists; the treatments received were reported as unhelpful in alleviation of symptoms [10].
Another Internet-based study that attempted to showcase the phenomenology of ORD obtained data from 253 subjects over a 3-month period in the year 2010. The participants were assessed using questionnaires that were specific to symptoms reported, along with the Depression Anxiety Stress Scales (DASS), Yale-Brown Obsessive–Compulsive Scale Modified for ORS (ORS-YBOCS), and Work and Social Adjustment Scale (WSAS). The age of onset of the illness was found to be an average of 21.1 years, more than half had a chronic course. The source of the odours were the armpits, feet, and breasts. The nature of the odours commonly reported related to stool, garbage, and ammonia. Eighteen percent had poor insight; 64% reported referential delusions. Almost all the patients spent time in repetitive rituals to reduce or hide the perceived odour. Women had greater illness severity. Severity was also associated with poor insight and impairment in work and social relationships [17].
Comorbidities
Major depression is frequently comorbid, both anxiety and depressive symptoms being prominent in about 40% of patients, often as a reaction to the ORD [10]. Up to 30% of the patients attempt self-harm, and more than half require hospitalization [6]. Other comorbid conditions include obsessive–compulsive disorder [18], social anxiety disorder [5], body dysmorphic disorder [10], and substance use disorders [10].
The frequency of occurrence of these comorbidities is depicted in Table 2.
Diagnosis
According to the ICD-11 criteria, the essential features required to diagnose olfactory reference disorder include the following:
-
“Persistent preoccupation about emitting a foul or offensive body odour or breath (i.e. halitosis) that is either unnoticeable or slightly noticeable to others such that the individual’s concerns are markedly disproportionate to the smell, if any is perceptible
-
Excessive self-consciousness about the perceived odour, often including ideas of self-reference (i.e. the conviction that people are taking notice, judging, or talking about the odour)
-
The preoccupation or self-consciousness is accompanied by any of the following: repetitive and excessive behaviours, such as repeatedly checking for body odour or checking the perceived source of the smell (e.g. clothing), or repeatedly seeking reassurance; excessive attempts to camouflage, alter, or prevent the perceived odour (e.g. using perfume or deodorant, repetitive bathing, brushing teeth, or changing clothing, avoidance of certain foods); marked avoidance of social or other situations or stimuli that increase distress about the perceived foul or offensive odour (e.g. public transportation or other situations of close proximity to other people)
-
The symptoms are not a manifestation of another medical condition and are not due to the effects of a substance or medication on the central nervous system, including withdrawal effects
-
The symptoms result in significant distress or significant impairment in personal, family, social, educational, occupational, or other important areas of functioning. If functioning is maintained, it is only through significant additional effort.”
Differential diagnosis
Several medical illnesses may present with a body odour that is objectively verifiable. Common ones include those related to the skin (hyperhidrosis), oral cavity (halitosis and dental abscesses), genital areas (rectal fistulae), and metabolic causes (trimethylaminuria). If the classical features of ORD are not met, then an underlying cause should be considered. Rarely, circumscribed ORD presentations may be a result of illnesses like temporal lobe epilepsy (TLE), arteriovenous malformations, and Parkinson’s disease. Associated olfactory hallucinations are rarely reported in ORD, and their presence must raise the suspicion of a TLE [19].
Psychiatric differentials include body dysmorphic disorder, obsessive–compulsive disorder, social anxiety disorder, and other delusional disorders of the somatic type. Rarely, a major depression with psychotic symptoms, bodily distress disorder, or an avoidant personality disorder can also present with ORD-like features [20].
A boundary with normality needs to be considered especially in cultures where fear of emitting offensive odours is a known entity. Both the ICD 11 and the DSM 5 allude to these cultural presentations. One such condition that is popularly described from Japan, Korea, and certain other cultures is the Taijin Kyofusho (Kyofu-fear and Taijin-interpersonal relationships). It is akin to social anxiety and is characterised by an extreme fear that one may offend, hurt, or embarrass others by awkward or unacceptable social behaviour, body movements, or appearance. These could include beliefs about blushing, eye contact, or offensive body odour. The one related to body odour is termed as Jikoshu-Kyofu (Jiko: oneself; Shu: odour, Kyofu: fear).
A study [21] undertaken in 2004 aimed to clarify the relationship between the Japanese Jikoshu-Kyofu and the Western ORD. A series of seven cases were analysed with specific emphasis on phenomenology and treatment. The researchers found that symptoms, insight, and drug response in the cultural variant were found to be identical to ORD, except when the onset of symptoms had been at a relatively younger age. They questioned the validity of the Jikoshu-Kyofu as a culturally distinctive disorder.
In yet another study from Japan [22], the authors attempted to trace a possible causal relationship among social anxiety, ORS, pathologic halitosis, and preoccupation with bodily smells. One thousand three hundred sixty female students (19.6 ± 1.1 years) were assessed using a self-administered questionnaire. Statistically significant differences in the results for ORS and social anxiety (P < 0.001) were found among the various severity grades of pathologic subjective halitosis. Participants with greater severity of pathologic subjective halitosis were found to be more preoccupied with body and mouth odours (P < 0.05). It was found that social anxiety has a direct influence on both pathologic subjective halitosis and ORS.
Olfactory reference disorder can be differentiated from regular or culture-bound concerns of body odour by the extent of preoccupation, frequency of related rituals carried out, and the severity of distress or interference the individual experiences because of his/her symptoms.
A recent paper [23] on a case series of four patients with ORS has presented some very interesting findings. The authors measured the olfactory function of the patients using a “University of Pennsylvania Smell Identification Test”. They found that all the patients had a genuine smell impairment, like that observed in patients who have dysosmia or phantosmia due to olfactory epithelium damage. Based on their novel findings, the authors speculated that patients with ORS may have an actual smell perception difficulty.
Assessment
A detailed clinical history taking will yield the symptoms necessary to make a diagnosis of olfactory reference disorder. If the presentation is atypical, relevant investigations need to be done to rule out underlying medical causes, e.g. an EEG when temporal lobe epilepsy is suspected.
A set of simple screening questions [24] can help uncover symptoms of ORD. “1. Are you very much concerned about your body odour? 2. Do you spend a lot of time worrying about your body odour? 3. Do you believe that other people perceive the body odour and take special notice of it? 4. Do you have urges to repeatedly do something to reduce the body odour? 5. Do you avoid certain situations due to this body odour? 6. Do these concerns affect your mood or daily life activities?”.
Rating scales that have been commonly employed include the Brown Assessment of Beliefs Scale (BABS) [25, 26] which is a seven item clinician administered instrument that assesses insight or delusional thinking across several psychiatric conditions, The Yale Brown Obsessive–Compulsive Scale modified for ORD [27, 28] which is a 12-item clinician-rated scale that assesses the severity of the ORD, and the Structured Clinical Interview for identifying disorders of the Obsessive–Compulsive Spectrum (SCID-OCSD) [29].
Treatment
The available literature on treatment of ORD is restricted mainly to case reports and case series. There are no randomised controlled trials on the use of psychotropics in ORD. There have been reports of specialists using antidepressants of various classes [30,31,32,33], both typical and atypical antipsychotics [34,35,36,37,38,39,40,41], as well as combinations of antipsychotics and antidepressants [42,43,44]. Various degrees of success have been reported with individual and combination therapy. However, there is no investigational proof of whether combined or sequential treatment leads to a more favourable outcome.
Regarding non-pharmacological treatment, case studies have documented response to various modalities, commonly behavioural techniques [45], eye movement desensitization and reprocessing [46], and cognitive behavioural therapy [47,48,49]. There have also been reports of patients improving with only psychotherapy [6].
There have also been case reports of patients showing improvement after a course of electroconvulsive therapy (ECT) was added to existing pharmacological management [50].
The systematic review [6] quoted in the article found that 33% of the patients improved with antipsychotic agents, while 55% responded well to antidepressant therapy. Only one in five cases showed symptom reduction with ECT, leucotomy did not have any effect on symptoms, and 78% improved with psychotherapy and 45% with varying combinations of treatment options. This lent further support to their argument that ORD must not be considered a delusional disorder.
Given the fact that the perception of the odour is considered a “physical” symptom by the sufferers, most of them may be reluctant to accept the need for psychiatric treatment. This is more pronounced when the ORS is associated with poor insight. However, most sufferers accept that the symptom is distressing and hampers their quality of life. Hence, the first step in offering treatment would be to establish a therapeutic rapport with the patient. The clinician needs to validate the patient’s symptom and, more importantly, the suffering endured. Patients are more likely to accept medications and therapy when offered to alleviate distress and anxiety rather than as a measure to stop the odour.
Prognosis
Data on prognosis of the condition is limited. Case reports and series have not measured treatment outcome or response in a uniform manner; some have relied on rating instruments, while others have simply commented on the symptoms that improved; each has used a different period from start of treatment to document response. Comorbidities have not been systematically examined while reporting response to treatment. In the 2011 systematic review [6], reduction in the olfactory symptoms was considered as recovery (complete or partial), while reduced preoccupation with the smell and interference in daily life activities was documented as improvement. Of the 84 cases assessed, 76 reported outcome data ranging from 2-week to 10-year follow-up period (average of 21 months). The authors found that 30% of the patients had recovered, 37% showed improvement, and 33% either continued to fare the same or worsened.
Conclusion
Olfactory reference syndrome is a commonly reported clinical condition which can present with varying degrees of insight. Sometimes, the severity of the conviction is almost delusional; at other times, it can present like an overvalued idea or with an associated obsessive component. Researchers have also attempted to view it as a dimensional concept, where concerns about normal body odour are intensified. Cultural variants have been described with components of associated social anxiety. Patients remain preoccupied with the perceived foul smell, often harbour ideas of reference, engage in repeated rituals to cleanse themselves of the odour, experience intense distress because of this condition, and suffer significant impairment in their social and occupational milieu. Like its nosological status, the treatment options also do not seem to be clear cut or conventionally defined. What appears to help the most is the establishment of a strong therapeutic alliance. Several classes of psychotropics alone and in combination have been tried with varying degrees of success, in addition to psychotherapy and electroconvulsive therapy. We need randomised controlled trials to get a clear understanding of effective treatment options.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were created or analysed in this review.
Abbreviations
- ORD:
-
Olfactory Reference Disorder
- ORS:
-
Olfactory Reference Syndrome
- ICD:
-
International Classification of Diseases
- DSM:
-
Diagnostic and Statistical Manual
- DASS:
-
Depression Anxiety Stress Scales
- ORS-YBOCS:
-
Yale-Brown Obsessive–Compulsive Scale Modified for ORS
- WSAS:
-
Work and Social Adjustment Scale
- OCD:
-
Obsessive–Compulsive Disorder
- BDD:
-
Body Dysmorphic Disorder
- TLE:
-
Temporal Lobe Epilepsy
- EEG:
-
Electro-encephalogram
- BABS:
-
Brown Assessment of Beliefs Scale
- SCID-OCSD:
-
Structured Clinical Interview for identifying disorders of the Obsessive–Compulsive Spectrum
- ECT:
-
Electroconvulsive therapy
References
Pryse-Phillips W (1971) An olfactory reference syndrome. Acta Psychiatr Scand 47:484–509
Tilley H (1895) Three cases of parosmia: causes, treatment, & C. The Lancet 146(3763):907–908
Videbech T (1966) Chronic olfactory paranoid syndromes. Acta Psychiatr Scand 42(2):183–213
Munro A (1988) Monosymptomatic hypochondriacal psychosis. Br J Psychiatry 153:37–40
Feusner JD, Phillips KA, Stein DJ (2010) Olfactory reference syndrome: issues for DSM-V. Depress Anxiety 27(6):592–599
Begum M, McKenna PJ (2011) Olfactory reference syndrome: a systematic review of the world literature. Psychol Med 41:453–461
Ren F, Zhou R, Zhou X, Schneider SC, Storch EA (2020) The latent structure of olfactory reference disorder symptoms: a taxometric analysis. J Obsessive Compuls Relat Disord 27:100583
Skimming KA, Miller CWT (2019) Transdiagnostic approach to olfactory reference syndrome: neurobiological considerations. Harv Rev Psychiatry 27(3):193–200
Osman AA (1991) Monosymptomatic hypochondriacal psychosis in developing countries. Br J Psychiatry 159(3):428–431
Phillips KA, Menard W (2011) Olfactory reference syndrome: demographic and clinical features of imagined body odour. Gen Hosp Psychiatry 33(4):398–406
Ferreira JA, Dallaqua RP, Fontenelle LF, Torres AR (2014) Olfactory reference syndrome: a still open nosological and treatment debate. Gen Hosp Psychiatry 36(6):760–763
Cruzado L, Caceres-Taco E, Calizaya JR (2012) Apropos of an olfactory reference syndrome case. Actas Esp Psiquiatr 40(4):234–8
Miranda-Sivelo A, Bajo-Del Pozo C, Fructuoso-Castellar A (2013) Unnecessary surgical treatment in a case of olfactory reference syndrome. Gen Hosp Psychiatry 35(6):683–684
Aydin M, Harvey-Woodworth CN (2014) Halitosis: a new definition and classification. Br Dent J 217(1):1–10
Jesus G, Gama Marques J, Durval R (2014) EPA-0909 – a review of olfactory reference syndrome about a series of clinical cases. Eur Psychiatry 29:1
Ross CA, Siddiqui AR, Matas M (1987) DSM-III: problems in diagnosis of paranoia and obsessive-compulsive disorder. Can J Psychiatry 32(2):146–148
Greenberg JL, Shaw AM, Reuman L, Shwartz R, Wilhelm S (2016) Clinical features of olfactory reference syndrome: an Internet -based study. J Psychosom Res 80:11–16
Zerzinski M, Burdzik M, Zmuda R, Debski P, Witkowska- Berek A et al (2023) Olfactory obsessions: a study of prevalence and phenomenology in the course of obsessive - compulsive disorder. J Clin Med 12(9):3081
Chen C, Shih YH, Yen DJ, Lirng JF, Guo YC, Yu HY, Yiu CH (2003) Olfactory auras in patients with temporal lobe epilepsy. Epilepsia 44(2):257–260
Lochner C, Stein DJ (2003) Olfactory reference syndrome: diagnostic criteria & differential diagnosis. J Postgrad Med 49(4):328–331
Suzuki K, Takei N, Iwata Y, Sekine Y, Toyoda T, Nakamura K, Mori N (2004). Do olfactory reference syndrome and Jiko-shu-kyofu (a subtype of Taijin-kyofu) share a common entity? Acta Psychiatr Scand 109(2):150–155.
Tsuruta M, Takahashi T, Tokunaga M, Iwasaki M, Kataoka S, Kakuta S et al (2017) Relationships between pathologic subjective halitosis, olfactory reference syndrome, and social anxiety in young Japanese women. BMC Psychol 5:7
Tallab H, Sell EA, Bromley SM, Doty RL (2023) A novel perspective on olfactory reference syndrome and associated specified obsessive-compulsive disorders. Ann Case Rep 8(1):1137–1142
Phillips KA, Castle DJ (2007) How to help patients with olfactory reference syndrome. Curr Psychiatr 6(3):49–65
Eisen JL, Phillips KA, Baer L, Beer DA, la Ata KD, Rasmussen SA (1998) The Brown Assessment of Beliefs Scale: reliability and validity. Am J Psychiatry 155:102
Phillips KA, Hart AS, Menard W, Eisen JL (2013) Psychometric evaluation of the Brown Assessment of Beliefs Scale in body dysmorphic disorder. J Nerv Ment 201(7):640–643
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL et al (1989) The Yale-Brown Obsessive-Compulsive Scale: I. Development, use, and reliability. Arch Gen Psychiatry 46:1006–1011
Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR et al (1989) The Yale-Brown Obsessive-Compulsive Scale: II. Validity Arch Gen Psychiatry 46:1012–1016
Du Toit PL, van Kradenburg J, Niehaus D, Stein DJ (2001) Comparison of obsessive-compulsive disorder patients with and without comorbid putative obsessive-compulsive spectrum disorders using a structured clinical interview. Compr Psychiatry 42:291–300
Brotman AW, Jenike MA (1984) Monosymptomatic hypochondriasis treated with tricyclic antidepressants. Am J of Psychiatry 141(12):1608–1609
Balaban OD, BOZ G, Senyasar K, Yazar MS, Keyvan A, Eradamlar N (2015) The olfactory reference syndrome treated with escitalopram: a case report. Marmara Med. J 28:120–122
Alhadi AN, Almaghrebi AH (2018) Challenges in diagnosis and treatment of olfactory reference syndrome: a case study. J Obsessive Compuls Relat Disord 19:23–28
Yoshimura R, Konishi Y, Okamato N, Ikenouchi A (2021) Letter to the Editor: Vortioxetine improved olfactory reference syndrome in a patient with major depressive disorder: a case report. Arch Clin Psychiatry 48(2):128
Ulzen TPM (1993) Letters to the Editor: Pimozide- responsive monosymptomatic hypochondriacal psychosis in an adolescent. Can J Psychiatry 38(2):154–155
Basu D, Bhagat A, Giridhar C, Avasthi A, Kulhara P (1990) Monosymptomatic hypochondriacal psychosis: a clinico-descriptive analysis. Indian J Psychol Med 13(2):147–152
Weintraub E, Robinson C (2000) A case of monosymptomatic hypochondriacal psychosis treated with olanzapine. Ann Clin Psychiatry 12(4):247–249
Nakaya M (2004) Letters to the editor: Olanzapine treatment of monosymptomatic hypochondriacal psychosis. Gen Hosp Psychiatry 26:164–169
Albers AD, Amato I, Albers MW (2018) Olanzapine improved symptoms and olfactory function in an olfactory reference syndrome patient. J Neuropsychiatr Clin Neurosci 30(2):164–167
Ikenouchi A, Terao T, Nakamura J (2004) A male case of monosymptomatic hypochondriacal psychosis responding to olanzapine: a case report. Pharmacopsychiatry 37:240–241
Reddy B, Nocera A, de Filippis R, Das S (2022) Two cases of olfactory reference syndrome treated with risperidone. Neuropsychiatric Invest 60(2):49–51
Elmer KB, George RM, Peterson K, Yokota AB, Langley AFB (2000) Therapeutic update: use of risperidone for the treatment of monosymptomatic hypochondriacal psychosis. Journal Am Acad Dermatol 43:683–686
Karia S, Shrivastava S, DeSousa A, Shah N (2013) Olfactory reference syndrome: a case report. Int J Sci Res 2(9):261
Ozten E, Sayar GH, Tufan AE, Cerit C, Dogan O (2013) Olfactory reference syndrome: treated with sertraline and olanzapine. Sch J Med Case Rep 1(2):44–46
Jegede O, Virk I, Cherukupally K, Germain W, Fouron P, Olupona T, Jolayemi A (2018) Case Report: Olfactory reference syndrome with suicidal attempt treated with pimozide and fluvoxamine. Case Rep Psychiatry 2018:1–3. Article ID 7876497. https://doi.org/10.1155/2018/7876497.
Milan MA, Kolko DJ (1982) Paradoxical intention in the treatment of obsessional flatulence ruminations. J Behav Ther Exp Psychiatry 13(2):167–172
McGoldrick T, Begum M, Brown KW (2008) EMDR & olfactory reference syndrome: a case series. J EMDR Pract Res 2(1):63–68
Haica C (2021) Olfactory reference syndrome: a case report. Mental Health Human Resilience Int J 5(2):1–7
Martin-Pinchora AL, Antony MM (2011) Successful treatment of olfactory reference syndrome with cognitive behavioral therapy: a case study. Cogn Behav Pract 18:545–554
Zantvoord JB, Vulink N, Denys D (2016) Cognitive behavioural therapy for olfactory reference syndrome: a case report. J Clin Psychiatry 77:9–10
Bhagat H, Bendre A, Dikshit R, DeSousa A, Shah N, Karia S (2017) Olfactory reference syndrome treated with electroconvulsive therapy. Annals Indian Psychiatry 1(2):129–131
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Both authors have contributed to the literature review and compilation of the article. The manuscript has been read and approved by both the authors, the requirements for authorship have been met, and each author believes that the manuscript represents honest work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Soman, S., Nair, R. Olfactory reference disorder—a review. Middle East Curr Psychiatry 30, 95 (2023). https://doi.org/10.1186/s43045-023-00367-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-023-00367-5